Battling Lymphatic System Disorders
Natural Max Health Improving Your Health: Essential Knowledge Series
As we explore further into the study of the lymphatic system and its related disorders, such as non-Hodgkin’s lymphoma and lymphedema, it is essential to underline the significance of maintaining its overall health. A compromised lymphatic system can result in severe health complications, so we must prioritize the system’s well-being.
So join me as I equip you with the knowledge to safeguard your health and empower your lymphatic system for a healthier life. Before we begin, let’s review some important terms and introduce new ones that will be helpful throughout this article.
- Lymph fluid – is a colorless and watery fluid made in the body. It surrounds all body tissues. Extra fluid from tissue in the body drains into and flows through small lymph vessels. This fluid is filtered through the lymph nodes and drains back into the bloodstream.
- Lymph node – small tissue lumps containing white blood cells that fight infections. They are part of your body’s immune system. They filter your lymph fluid.
- Lymphocytes – are white blood cells that are part of the immune system.
- Chyle – a milky fluid consisting of fat droplets and lymph. It drains from the lacteals of the small intestines into the lymphatic system during digestion.
- Lacteals – the lymphatic vessels of the small intestine that absorb digested fats.
- Gram-negative bacteria – are the most common primary pathogens. These organisms are often part of the normal flora but may become opportunistic.
- Pathogens – a bacteria, virus, or other microorganism that can cause disease.
- Endotoxin – is a toxin inside a bacterial cell and is released when the cell disintegrates. It is sometimes responsible for the characteristic symptoms of a disease.
Common Lymphatic System Disorders
The most common health issues associated with a poorly functioning lymphatic system are non-Hodgkins lymphoma, lymphadenitis, lymphangitis, lymphocytosis, and lymphedema.
Non-Hodgkins lymphoma is a type of cancer that begins in the lymphatic system, part of the body’s germ-fighting immune system. White blood cells called lymphocytes grow abnormally and can form growths or tumors throughout the body. Non-Hodgkins Lymphoma is a general category of lymphoma. Many subtypes fall into this category, but we will not dive into them in this article.
Lymphadenitis is an infection in one or more lymph nodes. There are two types of lymphadenitis: localized and general.
- Localized lymphadenitis – is the most common type. It involves one or just a few nodes that are close to the area where the infection started.
- Generalized lymphadenitis – occurs in two or more lymph node groups and may be caused by an infection that spreads throughout the bloodstream or another illness that affects the whole body.
Lymphangitis is inflammation of the lymphatic vessels. It’s a complication of skin infection, but it can also occur in people with certain types of cancer and other health issues.
Lymphocytosis is an increase in white blood cells called lymphocytes. Transient viral infections commonly cause it but can remain persistent in chronic infections such as hepatitis B. Although an unhealthy lymphatic system does not necessarily cause this condition, we thought it was worth mentioning.
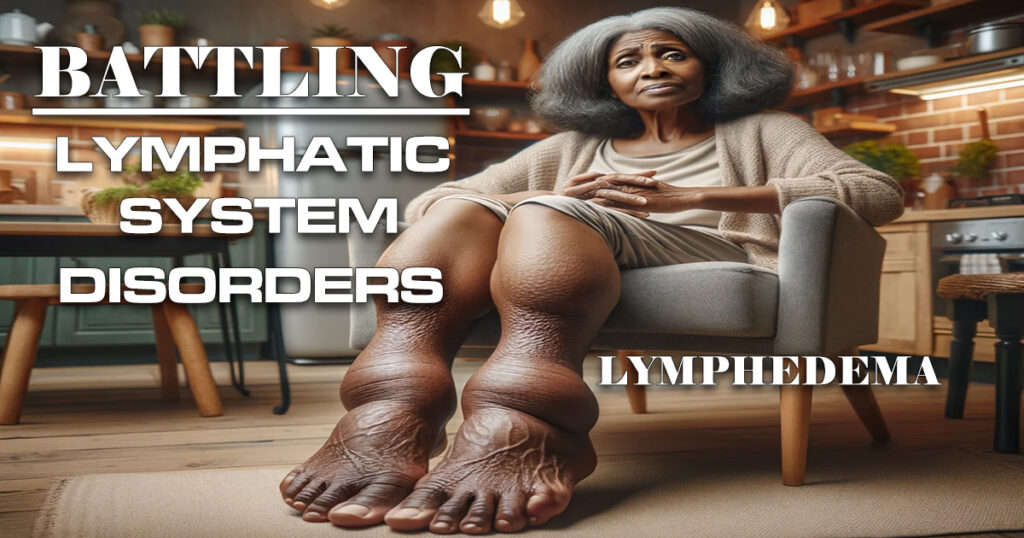
Lymphedema is caused by a blockage in the lymphatic system, one of the most common diseases of the lymphatic system.
“Lymphedema affects over 10 million Americans alone. That’s more people than those living with muscular dystrophy, ALS, and Parkinson’s combined.”
Sakinah Bellamy
Before we continue, let’s do a quick basic review of what the lymphatic system is so we can have a better understanding. Your lymphatic system is a group of organs, vessels, and tissues that protect you from infection and keep a healthy balance of fluids throughout your body. This network of organs, vessels, and tissues works together to collect excess fluid from your body’s tissues and return it to your bloodstream. Lymph is the term used to refer to the excess fluid. Lymphedema may occur when damage to the lymphatic system prevents lymph fluid from returning to the bloodstream. This causes lymphatic obstruction, evidenced by swelling and discomfort caused by a buildup of lymph fluid in the fatty tissues just under your skin.
Lymphedema vs. Lipedema and Edema
Lymphedema is often confused with lipedema and edema. So, before we continue, let’s clarify these conditions. Lipedema is a chronic condition that affects both sides of the body equally, consisting of fat and connective tissue that builds up in your legs, hips, bottom, and sometimes arms. It is sometimes considered a connective tissue disorder because collagen abnormalities affect how the fat cells expand. There are lymphatic abnormalities in the very early stages of lipedema and visible lymphedema swelling in the later stages, and according to some research, it is considered a fat disorder. This condition is more common in women and rarely affects men.
Edema
Edema can be a general term for acute swelling in the body that can affect any body part, but it is more likely to show up in the legs and feet. Medicines and pregnancy can cause edema. Edema swelling does not leave a mark when a finger is pressed into it. This is known as nonpitting. There are several stages of edema.
- Stage 0 indicates a normal extremity clinically but with abnormal lymph transport.
- Stage 1 is early edema, which improves with limb elevation.
- Stage 2 represents pitting edema that does not resolve with elevation.
- Stage 3 describes fibro adipose tissue, deposition, and skin changes. Fibroadipose tissue is a combination of fat and fibrous connective tissue. This abnormal tissue gradually grows into muscles and nerves, affecting their growth and formation. The fibrous portion can become tough and hardened, making it difficult for the joints to bend normally.
Lymphedema
On the other hand, lymphedema is a chronic and severe condition involving significant long-term edema fluid buildup. Lymphedema is a condition resulting from damage to the lymphatic system, characterized by swelling near the affected area. Unlike edema, lymphedema leaves an indentation when pressure is applied to it. Additionally, lymphedema has several stages.
- Stage 1 has abnormal flow in the lymphatic system with no signs or symptoms.
- Stage 2 is the accumulation of fluid with swelling. Swelling resolves with elevation, but pressing the area may leave a dent.
- Stage 3 is swelling that does not resolve with elevation. Pressing on the area no longer leaves a dent. There are changes in the skin with scarring and thickening.
- Stage 4 is called the elephantiasis stage, a large deformed limb. Additionally, the skin thickens with wart-like growth and extensive scarring.
The book “Lymphedema and Lipedema Nutrition Guide: foods, vitamins, minerals, and Supplements,” written by Chuck Ehrlich, Emily Iker, and Karen Louise Herbst, considers lymphedema a gut issue. Depending upon the source, this is plausible, considering that 30-50% of the lymphatic system is in the gut, and more than half of all lymph comes from the area. Gut bacteria impact lymphatic function as well as inflammation. So, maintaining a healthy gut goes hand in hand with maintaining a healthy and well-functioning lymphatic function.
Causes of Lymphedema
Long-chain fats pass through the lymphatic system as chyle. For this reason, diets high in fat increase lymph volume, which overloads central lymphatics, contributing to swelling and leakage. Reducing overall fat intake, including processed and fried foods, will decrease lymph volume.
Non-alcoholic fatty liver disease, which is common in overweight adults and children, causes the liver to produce 6-10 times as much lymph volume as a normal healthy liver. This causes swelling of the legs and abdomen and other health issues.
Overgrowth of E. coli and other gram-negative bacteria, Gram-negative bacteria release inflammatory endotoxins. Endotoxins decrease or stop lymphatic pumping action, which causes lymphatics to become leaky.
Gut permeability–changes in the gut lining that allow endotoxins and other toxins from the contents of the intestines to enter the bloodstream. Endotoxins decrease or stop lymphatic pumping. Contributing factors to gut permeability include gluten, a protein found in wheat, barley, or rye, alcohol, gut dysbiosis, liver disease, and maltodextrin and other food additives.
Lymphedema is commonly caused by the removal of lymph nodes or damage due to cancer treatment. Lymphedema often develops after breast cancer treatment, particularly in patients who received lymphadenectomy or radiation treatment. It usually affects the arm closest to the surgery but can also affect the breast, chest, underarm areas, or other body parts. The rate at which it develops varies per person, as it can develop quickly or slowly over several months.
Mutations in the genes responsible for the development of the lymphatic system can also cause lymphedema. The faulty genes cause the parts of the lymphatic system responsible for draining fluid not to develop correctly or not work as they should.
An infection, such as cellulitis, can sometimes cause lymphedema. Severe cellulitis can damage the tissue around the lymphatic system, causing it to become scarred,
Lymphatic filariasis is a parasitic disease caused by microscopic, thread-like worms that can also cause lymphedema. The adult worm only lives in the human lymphatic system and blocks lymph drainage.
Inflammation or medical conditions that cause tissue to become red and swollen can also damage the lymphatic system, including psoriasis and atopic eczema.
Immobility – movement and exercise increase lymph drainage. Therefore, reduced movement can lead to lymphedema.
Venous diseases – diseases that affect blood flow through the veins can cause lymphedema.
Obesity, trauma, and injury – are other factors. In some cases, lymphedema can result from damage to the lymphatic system due to accidental injury.
Treatments for Lymphedema
Treatment for lymphedema depends on the severity and the extent of the condition. According to most research, there is no cure, so prevention is paramount. If you have or believe that you have lymphedema, particularly in advanced stages, please see your doctor immediately because surgery such as liposuction may be necessary. If your doctor needs more information about this condition, kindly ask for a referral. Whatever stage you may be in, you can take action to control and manage this disease. I have listed some non-surgical therapies that can reverse or reduce some symptoms.
Diet – First and foremost, diet will always be essential. As we pointed out previously, diets high in fat, processed food, fried food, carbohydrates, gluten, and alcohol can play a significant role in damaging your lymphatic system. So, it’s only reasonable that reducing or eliminating these foods will improve your health. Increase inulin fiber from food sources or supplements. Eat fermented food every day. Decrease omega-6 fats from grain-fed animal products, corn, soy, and processed foods, and increase omega-3 fats from wild fatty fish, walnuts, flaxseeds, and other sources or supplements. Increase arginine from foods such as fish, non-GMO soy, beans, lentils, and nuts, including almonds and walnuts. Increase foods rich in nitrate and nitrite, such as leafy green vegetables and fruits. Minimize fats, fructose, and other sugars, and refined carbohydrates.
Exercising or moving your body – helps restore flexibility and strength and improves drainage. Engaging in rebounding, walking, swimming, and stretching exercises is highly advisable. These forms of exercise are great for maintaining good health.
Manual lymph drainage – is a hands-on technique that differs from standard massage by orienting the lymphedematous fluid to proper functioning.
Arm pump – Applying an arm pump often helps to increase the fluid flow in the lymphatic vessels and keeps fluid from collecting in the arm.
Bandage – Wearing a customized compression sleeve or elastic bandage may help to prevent fluid accumulation.
Compression therapy – involves using bandages, wraps, or compression garments to apply varying pressure levels to the affected area.
Skin care – Following preventive measures, such as good skin care, is essential to protect the affected area from infection.
Gut health – as stated previously, an improper balance of bacteria in the gut can also lead to lymphedema. So, maintaining gut health is also essential.
In Closing
Although research suggests that there is no cure for lymphedema, in my opinion, depending on how the condition develops, it may be reversible. For example, if lymphedema develops due to poor diet or poor gut health, correcting those factors will likely reverse the damage. However, I don’t have any evidence to back this up; it is only an opinion.
If you suffer from lymphedema, don’t let anyone determine your fate and tell you it’s not reversible and that you will never heal. Be your own doctor, take steps to improve your health, and see what happens. You can change your diet, improve your gut health, drink more water to remove toxins, get lymphatic massages, or even exercise to improve lymph flow. If you don’t like exercising, you can listen to music and dance like no one is watching. What do you have to lose besides some excess fluid?
Recommended reading: Lymphedema and Lipedema Nutrition Guide: foods, vitamins, minerals, and supplements by Chuck Ehrlich, Emily Iker, and Karen Louise Herbst.
Related Links
Signs of an Unhealthy Lymphatic System and What To Do
Lymphatic System & Digestion: Unveiling the Hidden Link
The Vital Dance: Blood & Lymph Circulation Harmony
Unlocking the Mysteries of Your Body: A Beginner’s Guide to the Lymphatic System
The Ultimate Health Sheild: Unleash Your Immune System Superpowers
